Okay. So let me preface this by letting you all know how excited I was by this article (must log in to Science magazine to view full article), on a 1-10 scale. I think I'm circling around an 8.
Anyway, so I've always assumed higher mRNA levels are directly correlated with increased gene expression, and therefore higher levels of the protein coded by that gene. Right?
Welp. Apparently, according to researchers at Harvard and the University of Toronto, that's not necessarily true, due to differences in how long mRNA and proteins last in cells. The study utilized a YFP (yellow fluorescent protein) and single molecule FISH which allowed the researchers to quantitatively assess levels of gene expression and mRNA molecules expressed by the YFP-tagged genes. Being that they used gram-negative E. coli cells for the purpose of this study, they controlled for the differences in bacterial gene transcripts by "providing quantitative analyses of both abundance and noise in the proteome and transcriptome on a single-cell level", says Taniguchi, et al. As Sunney Xie comments, "this provides a cautionary note for people who want to do single cell mRNA-profiling".
The main finding of this study is that a single cell's protein and mRNA copy number for any given gene are uncorrelated. As the authors wrote, the study highlights the disconnect between proteome and transcriptome analyses of a single cell. It's also important in understanding how cells coordinate the expression of proteins that work together, such as multi-subunit proteins or proteins that serve within metabolic cycles.
July 30, 2010
July 26, 2010
hipsters: not only do I not like you, but your transcriptomes don't either.
 |
| naturopathicyoga.com |
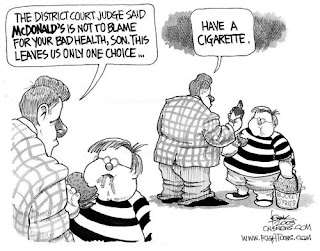
Genome-wide quantitative transcriptional profiles taken from 1,240 subjects in the San Antonio Family Heart Study* (included ~300 current smokers) identified 323 unique genes whose expression pattern levels were significantly correated with smoking behavior! (provisional abstract) These genes have been implicated in immune response, cancer and cell death. The study has also suggested that smoking cigarettes can alter the expression of hundreds of white blood cell genes. As an article on GenomeWeb points out, "a comprehensive picture of how smoking affects the body has been difficult because cigarette smoke contains thousands of compounds that seem to act throughout the body".
With the current craze in the genomics world to understand how, and to what extent, environmental factors influence an individual's gene expression pattern, these findings are especially exciting. Smoking is considered an environmental factor, and we can see that just in this one study, it affects the expression of hundreds of genes and gene networks. It would be interesting to somehow assess how second-hand smoke exposure affects the genomes of individuals who have been exposed to second-hand smoke on a regular basis. I'm sure a study like that would push some places (coughvassarcough) to more rapid non-smoking policy. Speaking of, today Vanderbilt students found out that come Fall, their campus would be strictly non-smoking, and smoking would therefore be designated to specific locations on campus (where all the hipsters can gather and indulge). Let's get a move on it Vassar.
*Potential sample bias considering subjects of the study are involved in a Heart Study? Could gene expression profiles be different since subjects are in hypertension/obesity experiments? This study should probably be re-done with a random cohort, controlled for gender/SES/family history/age/smoking frequency, with equal numbers of smokers and non-smokers.
July 25, 2010
MS: Vascular or Neurological?
As I have mentioned previously, Multiple Sclerosis has always been defined as a neurological autoimmune disease that affects the central nervous system. Well, there is now reason to speculate that MS is actually (at least partially) induced by attenuated veins in the neck and chest that block the proper drainage of blood from the brain. Dr. Paolo Zamboni, an Italian vascular surgeon who has been accredited with this vascular theory of MS, has been advocating the usage of a "liberation procedure" in which a balloon is inserted into one of these narrowed veins and inflated, with the intent of thickening the blood passageway and ameliorating blood flow from the brain.
This idea is particularly intriguing to me, considering the study is taking place in the Jacobs Neurological Institute at Buffalo General Hospital, steps away from where I worked this Summer. We even discussed the possible ethical dilemmas associated with the study in a staff meeting last week. Although I tend to steer clear of the New York Times for science updates, this one article does a great job of explaining what is happening in Buffalo and what issues some people have with the experimentation.
Personally, I think this study is a great idea. I understand the risk behind the surgical procedure, but all the patients involved have consented, and understand the risk behind undergoing the surgery. Although the study is double-blind, and some patients will undergo a sham surgery (balloon is inserted but taken out without being inflated in the target vein), patients were notified prior to consenting that they could be undergoing a sham surgery in which they would not be receiving the potential therapy. To be honest, a lot of the research happening at the JNI is focused on how we can reduce the side-effects of the already existing MS therapies. Antigenicity of Copaxone, Rebif and Interferon-beta have been worrisome, and, Tysabri - although effective - has been associated with increased risk for PML, an incurable, untreatable and sometimes fatal brain infection. I think patients who have been diagnosed with MS and are suffering are for the most part unopposed to a potential new treatment, that most likely does not have any more risks than any other surgical procedure might have. Furthermore, the experimental phase of the study has not even begun yet. Right now, doctors are simply performing the procedures and monitoring patients to make sure that the surgery itself is not harming them. I believe the first procedures took place about a month ago, and it will be a few months until the experimental phase of the study begins.
I myself do not know if I believe MS is a vascular disease, but I do not see any harm in finding out more. Should this study be successful in targeting the narrowing of blood passageways as a direct cause or exacerbating factor of MS, it will lead to a wide array of new (and most likely less risky) therapeutic options. From a genomics point of view, it will help us identify new genes and loci that might be vital on the pharmacogenomics side of things. I do not know whether or not this is included in the study - but I do hope that after the conclusion of the study, patients who had unknowingly received the sham procedure are entitled to the actual liberation surgery if they so choose.
Now, I don't consider myself anywhere close to an MS expert, but based on what I do know, I would expect to find an association between severity of symptoms/relapses and vein narrowing. However, I think there is too much evidence to point to MS as a neurologically-driven autoimmune disease. All in all, if you couldn't tell by the frenzied state of my writing in this post, I'm pretty freakin' excited by the potential of the study.
This idea is particularly intriguing to me, considering the study is taking place in the Jacobs Neurological Institute at Buffalo General Hospital, steps away from where I worked this Summer. We even discussed the possible ethical dilemmas associated with the study in a staff meeting last week. Although I tend to steer clear of the New York Times for science updates, this one article does a great job of explaining what is happening in Buffalo and what issues some people have with the experimentation.
Personally, I think this study is a great idea. I understand the risk behind the surgical procedure, but all the patients involved have consented, and understand the risk behind undergoing the surgery. Although the study is double-blind, and some patients will undergo a sham surgery (balloon is inserted but taken out without being inflated in the target vein), patients were notified prior to consenting that they could be undergoing a sham surgery in which they would not be receiving the potential therapy. To be honest, a lot of the research happening at the JNI is focused on how we can reduce the side-effects of the already existing MS therapies. Antigenicity of Copaxone, Rebif and Interferon-beta have been worrisome, and, Tysabri - although effective - has been associated with increased risk for PML, an incurable, untreatable and sometimes fatal brain infection. I think patients who have been diagnosed with MS and are suffering are for the most part unopposed to a potential new treatment, that most likely does not have any more risks than any other surgical procedure might have. Furthermore, the experimental phase of the study has not even begun yet. Right now, doctors are simply performing the procedures and monitoring patients to make sure that the surgery itself is not harming them. I believe the first procedures took place about a month ago, and it will be a few months until the experimental phase of the study begins.
I myself do not know if I believe MS is a vascular disease, but I do not see any harm in finding out more. Should this study be successful in targeting the narrowing of blood passageways as a direct cause or exacerbating factor of MS, it will lead to a wide array of new (and most likely less risky) therapeutic options. From a genomics point of view, it will help us identify new genes and loci that might be vital on the pharmacogenomics side of things. I do not know whether or not this is included in the study - but I do hope that after the conclusion of the study, patients who had unknowingly received the sham procedure are entitled to the actual liberation surgery if they so choose.
Now, I don't consider myself anywhere close to an MS expert, but based on what I do know, I would expect to find an association between severity of symptoms/relapses and vein narrowing. However, I think there is too much evidence to point to MS as a neurologically-driven autoimmune disease. All in all, if you couldn't tell by the frenzied state of my writing in this post, I'm pretty freakin' excited by the potential of the study.
miRNA for noobs
MicroRNA is one of the coolest things ever. If you don't know what it is, do yourself a favor and at least read the Wikipedia article about it. Or take 1:23 to watch a sweet animation. I'm willing to bet miRNA and RNA interference studies hold the key to many of the ambiguities in clinical research.
summer in Buffalo 2010
As of yesterday, I completed a 7-week research internship at the Jacobs Neurological Institute in Buffalo. If you asked me what I knew about Multiple Sclerosis on June 5th, I would have told you what we had touched upon in Physiological Psychology - basically that it was an autoimmune disease that severely impacts the central nervous system. Over the past month and a half, my knowledge of the disease - and the field of clinical research in general - has been expanded by leaps and bounds.
My original assignment was to assess the recent advancements in the field, and the future directions that research should take. At the conclusion of the internship, the only material I could physically produce was a 1500-word review paper on the pharmacogenomics and pharmacogenetics of MS. My initial feeling was one of disappointment - I couldn't believe that it had taken me 5 weeks to write 1500 words. But when I realized how far I had come in my understanding of the pharmacogenomics of MS, my feelings of disappointment were mollified.
I've read - and understood (!!) - between 30 and 40 primary research papers written since the beginning of 2010 on everything from miRNA (micro RNA) assays, post-translational modification studies, GWAS (genome-wide association studies) to the use of animal models with EAE (experimental autoimmune encephalomyelitis). These are just some of the ways in which researchers have been attempting to further understand both the susceptibility and severity factors of MS in the past few years.
While there are so many interesting things I have learned - some of which I will post about at a later date - I think the most prevalent and intriguing pieces to the MS puzzle are the links we have made to the individual genome. Given that I am boarding a flight back home in a mere 5 hours, I only have the time to talk about one of my favorites for now:
For the past few years it's been widely accepted that, the HLA-DRB1 gene, encoding for the HLA class II histocompatibility antigen DRB1-9 beta chain protein, is associated with MS susceptibility. Just this year, researchers have furthered this belief by proving that the presence of oligoclonal bands in the CSF is significantly associated with the presence of the HLA-DRB1 genotype in a West Australian cohort (Wu, et al. 2010). This was the first study ever to show that HLA-DRB1 allele interactions and dose-effects influence the frequency of oligoclonal bands**. Wu, et al. went a step further to target HLA-DRB1*1501 as not only a strong determinant of MS risk, but also as a predictor of MS severity as measured by the MSSS (MS Severity Score). Furthermore, the HLA-DRB1*1201 allele was linked to less severe cases of the disease. Another study (Zivkovix, et al. 2009) concluded that, specifically, the tag SNP for HLA-DRB1*1501 (rs313588) is present in significantly higher frequencies in MS patients compared to control subjects.
Before heading off to sleep in anticipation of my long-awaited departure from Buffalo, I think it's worth it to mention another study which ties into the above discoveries. In 2008, Hoffman et al. found that the HLA-DRB*1401 and HLA-DRB1*0408 alleles are strongly associated with the development of antibodies against interferon-beta MS therapy. I wonder if this means that they would both be linked to more severe cases of MS? Would that mean that the HLA-DRB*1501 allele also has more antigenic properties in response to IFN-beta? Cool stuff. For a genomics nerd at least...
 |
| **http://library.med.utah.edu/kw/ms/mml/ms_oligoclonal.html The presence of OCBs in the CSF usually indicates immunoglobulin production in the CNS, suggesting a case of MS in the patient (as seen on the right) |
Subscribe to:
Posts (Atom)